 Robotic surgery does not eliminate the need for human surgeons, but some feel that it does make the humans better surgeons. The robot can help to eliminate human errors in surgery, making delicate procedures more precise.
Robotic surgery does not eliminate the need for human surgeons, but some feel that it does make the humans better surgeons. The robot can help to eliminate human errors in surgery, making delicate procedures more precise.
There is great debate about how much robotic surgery helps when compared to traditional surgery, but there is no questions that many doctors and patients want this technology available.
Robots Used in Orthopedics
Robots can perform, or help perform, a variety of tasks during surgery. In orthopedics, most robotic applications have focused on joint replacement surgery.
The primary goal during surgery to replace a joint is to properly position the prosthetic joint with a perfect fit, proper alignment, with restoration of joint function.
In fact, the longevity and function of joint replacements has been shown to be related to how well the surgery is performed. It cannot be understated how important this factor is in determining the success of joint replacement. I often hear patients focusing on variables such as the type or brand of implant, when in actually, the most important variable is probably how well the implant is placed in the body. A great implant will not overcome poor surgical technique. Robots can help to control the insertion of joint replacements in the body.
In hip and knee replacement, robots have been used to help guide appropriate bone cuts to accommodate the implanted joint. Robots can also be used to help navigate the anatomy to ensure proper alignmentof an implanted joint.
Success of Robotic Surgery
There have been studies to investigate the success of robotic surgery.
Most of the research is sponsored by the companies investigating the new technology, so there are questions about the quality of some of these studies.
The general theme of the research has shown that robotic surgery may help improve the consistency with which surgeons implant joint replacements. However, there is no research that clearly demonstrates an improvement in how long joint replacements last or how well they function. Most advocates of robotic applications in orthopedic surgery are basing their recommendations on theoretical benefits rather than on actual data.
Problems With Robots
As stated, robotic surgery is a rapidly growing area of surgery, but there is much left to be learned. Robotic surgery is very expensive, and with little demonstrated benefit, many question if this is an appropriate expense.
I use the robot for selected patients including partial knee replacements, and patients who have a deformity requiring a hip replacement.

 The use of an antibiotic pill prior to dental work has been thought to lower this risk. In 2013, The American Academy of Orthopaedic Surgeons and The American Dental Association worked together to create guidelines for this situation. The work group reviewed the available published data to try and synthesize recommendations for patients and practitioners. Unfortunately, there is not a large amount of quality data.
The use of an antibiotic pill prior to dental work has been thought to lower this risk. In 2013, The American Academy of Orthopaedic Surgeons and The American Dental Association worked together to create guidelines for this situation. The work group reviewed the available published data to try and synthesize recommendations for patients and practitioners. Unfortunately, there is not a large amount of quality data. A commonly asked question by those seeking a joint replacement is how soon can I fly after the surgery?
A commonly asked question by those seeking a joint replacement is how soon can I fly after the surgery? Several treatments for osteoarthritis exist, including exercise, weight control, bracing, nonsteroidal anti-inflammatories, Tylenol, cortisone shots and viscosupplementation, a procedure that involves injecting a gel-like substance into the knee to supplement the natural lubricant in the joint. A new treatment that is being studied by a small number of doctors is PRP injections. PRP, which is produced from a patient’s own blood, delivers a high concentration of growth factors to arthritic cartilage that can potentially enhance healing.
Several treatments for osteoarthritis exist, including exercise, weight control, bracing, nonsteroidal anti-inflammatories, Tylenol, cortisone shots and viscosupplementation, a procedure that involves injecting a gel-like substance into the knee to supplement the natural lubricant in the joint. A new treatment that is being studied by a small number of doctors is PRP injections. PRP, which is produced from a patient’s own blood, delivers a high concentration of growth factors to arthritic cartilage that can potentially enhance healing. The good news is that studies show that common types of knee replacements can last more than 20 years. One recent study on long-term outcomes of a commonly used knee replacement found the implant to still be functioning in 96% of patients 20 years after being implanted.
The good news is that studies show that common types of knee replacements can last more than 20 years. One recent study on long-term outcomes of a commonly used knee replacement found the implant to still be functioning in 96% of patients 20 years after being implanted. A total hip replacement is a big surgery, and therefore deciding to have the surgery done is a big decision. Here are some signs to look for to help you decide if the time is right, or not right, for hip replacement surgery.
A total hip replacement is a big surgery, and therefore deciding to have the surgery done is a big decision. Here are some signs to look for to help you decide if the time is right, or not right, for hip replacement surgery. Healthy patients who undergo total hip replacement (THR) can be fast tracked to be discharged in two days compared with the standard three to six days, according to a study by researchers at Hospital for Special Surgery (HSS) in New York City. The study could help cut down on hospital-acquired infections, reduce hospital costs and improve patient satisfaction.
Healthy patients who undergo total hip replacement (THR) can be fast tracked to be discharged in two days compared with the standard three to six days, according to a study by researchers at Hospital for Special Surgery (HSS) in New York City. The study could help cut down on hospital-acquired infections, reduce hospital costs and improve patient satisfaction. Results of a new retrospective observational study showed patients with knee osteoarthritis who were treated with intra-articular hyaluronic acid had a longer time to knee arthroplasty compared with patients who did not receive the injections.
Results of a new retrospective observational study showed patients with knee osteoarthritis who were treated with intra-articular hyaluronic acid had a longer time to knee arthroplasty compared with patients who did not receive the injections.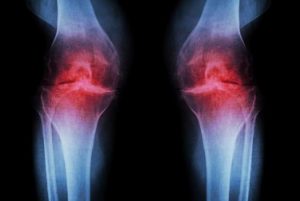 Depending on the location of osteoarthritis, a patient’s driving capability can be impaired and can show significantly increased total braking distance, according to recently published results.
Depending on the location of osteoarthritis, a patient’s driving capability can be impaired and can show significantly increased total braking distance, according to recently published results. Hip replacement surgery has long been used to treat hip arthritis in elderly patients. However, concerns arise when a patient in his 40s, 50s, or younger, has severe arthrtis that is not relieved with non-operative treatments. Once reserved for elderly patients, hip replacement surgery is now becoming more common in the younger, active population.
Hip replacement surgery has long been used to treat hip arthritis in elderly patients. However, concerns arise when a patient in his 40s, 50s, or younger, has severe arthrtis that is not relieved with non-operative treatments. Once reserved for elderly patients, hip replacement surgery is now becoming more common in the younger, active population.